
By collaborating closely with a maxillofacial surgeon, PDR improved the speed, predictability and accuracy of this critical, complex procedure. The patient had a bone tumour which was invading the orbit, applying pressure to the optic nerve and threatening their eyesight.
The surgeon, Mr Satyajeet Bhatia from University Hospital of Wales in Cardiff approached PDR to assist in establishing a safe surgical plan; translate this plan robustly into the realities of the operating theatre using custom surgical cutting guides; then reconstruct the functionally and aesthetically-critical defect using a digitally designed and 3d-printed custom titanium multi-part implant.
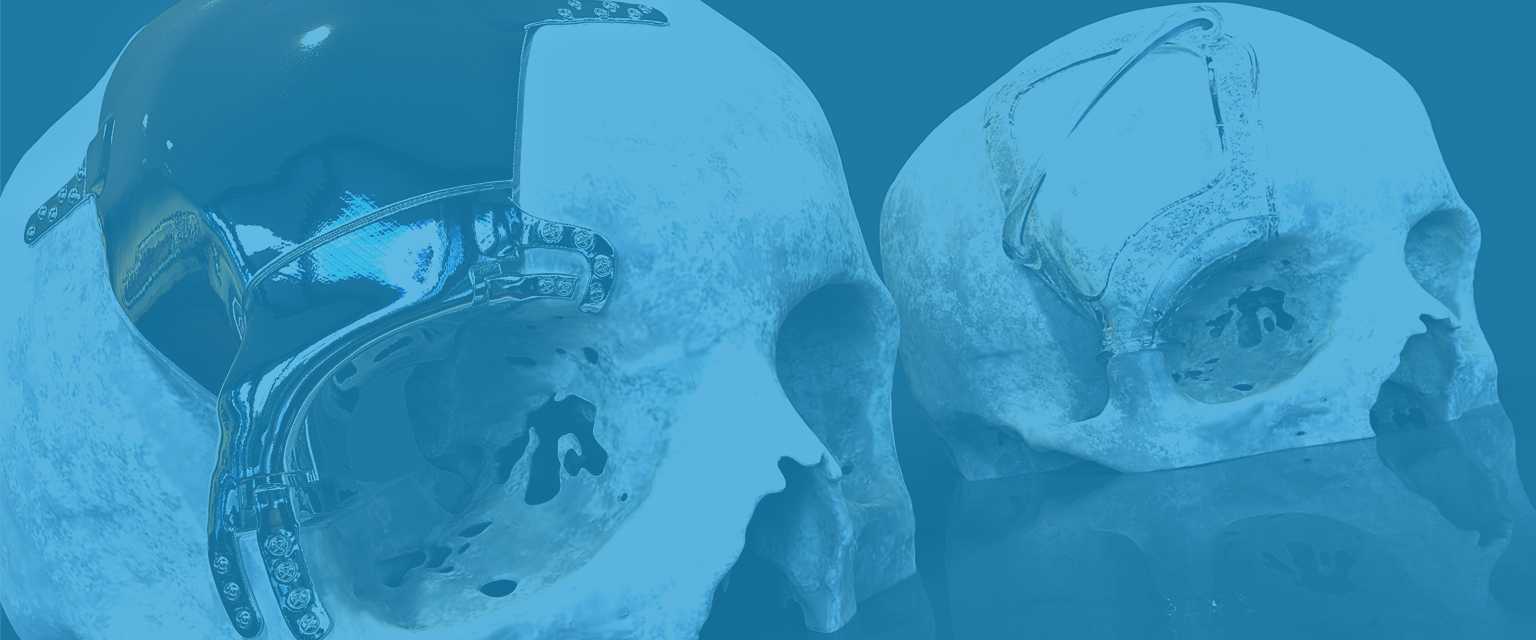
Initially, PDR rapidly provided a medical model of the patient’s cranium from their most recent scan data. Mr Bhatia used this as a tactile and visual aid during discussions with neurosurgical and ophthalmology colleagues. Together, they marked the extents of their desired tumour excision margin. PDR design engineers translated this margin onto a 3D virtual model of the patient and designed surgical cutting templates which located predictably, securely and recurrently onto consistent anatomical landmarks. The guiding ledge was adjusted to dictate the saw-blade angle and therefore avoid the critical frontal sinus border.
Then, based on a mirrored version of the patient’s healthy contralateral anatomy, a three-part reconstructive implant was designed and modelled to restore the aesthetic and mechanical functionality in the area of excised bone. The three-part solution was selected for its insertion flexibility. With the main orbital rim component screwed into position, the (undercut) superior orbit section became easier to insert thanks to the smaller size. The largest, simplest, frontal / temporal cranioplasty portion completed the reconstruction.
A gap was left between all components and the defect edge – to accommodate any small misalignment of the components in-theatre. Long tabs for fixation were chosen – to account for the potential of using larger excision margins than originally planned (in the event of tumour growth since the most recent scan). Lips on the orbital rim component were included to support secure assembly, gap filling between components, and (via cut-outs to accommodate neighbouring tabs) correct orientation of each piece.
In surgery, thanks to the careful consideration and collaboration behind each component, each guide and implant worked as planned – without delays or technical faults. Surgery time was reduced, the accuracy of the reconstruction (relative to traditional methods) improved, and the predictability of the procedure increased.
"By using these devices, surgery is now quicker and more accurate, patient outcomes are improved, and patients typically require fewer surgical interventions. This is because the research undertaken by PDR has negated much investigatory surgery, as planning and implant development now happens in a digital environment based on medical imaging data".
MR BHATIA
